A Simplified introduction to the Human Spine
Please Read this before reading specific surgical procedures

The spine (vertebral column) is made up of several bones called vertebrae which are stacked one upon another. Each vertebra is joined to the vertebrae above and below by two pairs of joints called the facet joints situated on the two sides. The typical vertebra has a solid body in front and two plate-like structures on two sides at the back called laminae. The laminae meet in the midline to form a protrusion, the spinous process, which can be felt through the skin of the back. On the two sides each lamina is joined to the body of the vertebra by a short bony stud called the pedicle, thus completing a bony ring. These rings inside each vertebra join together to form a tube called the spinal canal through which passes the spinal cord and the nerve roots.
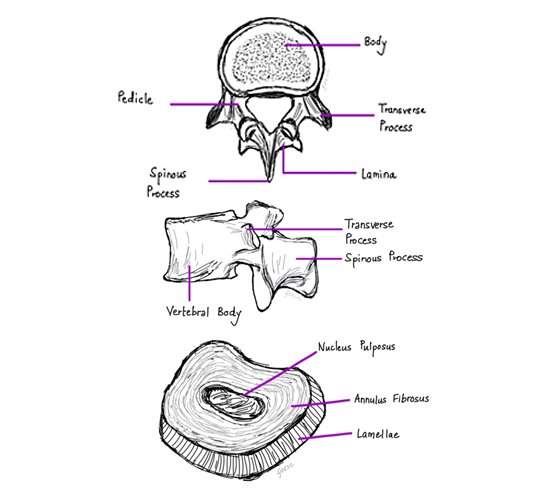
A small gap, the intervertebral foramen, is present in between the adjacent pedicles for the passage of the nerve roots. These nerve roots are the connections that carry all sensations from the body to the brain and also bring commands from the brain to muscles resulting in movement. In between two adjacent vertebral bodies there is a strong rubber like tissue (Cartilage), resembling a washer, called the intervertebral disc. The nerve root in the intervertebral foramen lies just behind the disc. A disc has a stronger outer part called the annulus fibrosus and a softer jelly-like central part called the nucleus pulposus. When a patient has a prolapsed disc, the central soft part of the disc bulges out and can press on the nerve root/s.
Operation Theatre
Some Common Operative Procedures
Cervical Spine (Neck):
Cervical radiculopathy is a condition in which there is compression of the nerves that connect the upper limbs with the spinal cord at the neck. Patients usually present with neck pain which spreads to the shoulders and arms. Pain may be associated with tingling, numbness, pins and needles sensation, and weakness of the upper limbs. If neglected there may be weakness with wasting and loss of sensation of the limbs and even complete paralysis. The commonest cause of such compression of the nerves is a degenerative condition of the spine referred to as Cervical Spondylosis. In this condition changes occur in the intervertebral discs including loss of height and loss of its capacity to hold water. The body responds to these changes by forming extra bone, called spurs, around the affected disc to strengthen it. The loss in disc height and the bony spurs collectively narrow the area and pinch the nerves. Protrusion of parts of the degenerated disc can also cause or aggravate the pressure on the nerves (slipped disc/ prolapsed disc).

FAQs:
- How many days do I need to stay in Hospital?
Patients are usually admitted to the hospital a day before the surgery. After the surgery, patients will be up walking around within the first day after surgery and throughout the rest of the hospital stay period. If surgery is being done for arm pain due to nerve root compression, this pain is usually significantly improves shortly after surgery. If weakness or numbness was present prior to surgery these symptoms may take longer to recover. Patients are usually observed for 2 days and discharged on the 3rd day. This allows us to make sure that your pain is well-controlled on oral medications prior to discharging home and to make sure that you are able to swallow regular food comfortably. - How long does this surgery take?
The length of surgery depends on each individual patient’s circumstances and diagnosis. Sometimes patients may need more than one level decompression and fusion. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. These complications are very few and quiet rare. The risks of surgery include difficulty in swallowing, change of voice, infection, pain that persists after surgery, potential nerve or spinal cord damage and tear of the covering around the nerves. There is also a risk that the level above or below a fused level will have an accelerated rate of degeneration. Around 10% of patients will have some temporary complications most of which are treatable and improve in further course. Only 1% of patient will have permanent complications. The risks of anaesthesia are largely based on the patient’s general physical health which usually investigated by the anaesthetist prior to your surgery. The treating surgeon and anaesthetist will discuss these risks in further detail at your pre-operative visit. - What is the follow up protocol?
Follow up visit is scheduled at 1 month, 3 month, 1 year and 2 year. In each successive follow up, patient’s restriction is relaxed and he/she is encouraged to join his/her duties, do all active exercises and get back to normal life. - Will I need a cervical collar after surgery?
The style of brace and length a patient must wear it depends upon the specifics of surgery and various other factors. Most of the time for a standard single level anterior cervical Discectomy and Fusion, brace is not required. Instead patients are encouraged to do all neck exercises. - How much pain will I have, and will I receive pain medications?
Each patient has different pain tolerance. Before the discharge from hospital, the goal is to have your pain controlled on oral medications only. - Do I need to take any other medications after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After the discharge from hospital, patient is supposed to keep this dressing as dry as possible. If you notice any soakage of dressing then you should call to our helpline number to let us know. Since we do the subcuticular (below the skin) closure using dissolvable stitches there is no need of removal. - Do I need to do the physical therapy after surgery?
Patient is encouraged to do all exercises which he/she was taught during the hospital stay. Patient can coordinate with our dedicated spine physiotherapy team for other queries.

Cervical spondylotic myelopathy (CSM) refers to disturbances in the functioning of the spinal cord due to compression by bony outgrowths, ligaments becoming bony, or by large disc herniations. The normal wear-and-tear effects of aging can lead to a narrowing of the spinal canal squeezing the spinal cord. Patients may complain of neck pain, tingling-numbness and weakness of any or all of the limbs. Subtle symptoms like difficulty in buttoning shirts, dropping things, loss of balance while walking, changes in handwriting and urinary disturbances may be early warnings. These symptoms usually begin after the age of 50 and unless treated energetically, many people will have steady progression of their disease till they are completely crippled.
FAQs: Please see Anterior Cervical Discectomy and Fusion (ACDF) (above)....

FAQs:
- How many days do I need to stay back in Hopsital?
Patients are usually admitted to the hospital a day before the surgery. After the surgery, mobile and ambulatory patients will be up and about in a day or two after operation. If weakness or numbness was present prior to surgery these symptoms may take longer to recover. Most patients will be fit to go home in a week after a course of intensive physiotherapy. - How long does this surgery take?
The time taken for surgery depends on each individual patient’s physical structure (e.g. height and weight) and diagnosis. The actual time needed for operation also depends on the number of levels to be decompressed and fused. - Are there risks involved in this surgery?
There are risks and benefits in every medical or surgical intervention. Complications are rare, and, if they occur, usually mild. The risks of surgery include difficulty in swallowing, hoarseness of voice, infection, and persistent pain after surgery. Relatively serious complications like nerve or spinal cord damage leading to weakness of hands and feet, and tear of the covering around the nerves leading to leakage of fluid with wound healing problems are very infrequent. The levels above and/or below the operated level may have an accelerated rate of degeneration. Around 10% of patients will have some complication most of which are treatable and improve with time. Less than 1% will have permanent complications. The risks of anaesthesia are largely based on the patient’s general health which will be investigated and managed by the anaesthesiology team. The treating surgeon and anaesthesiologist will discuss these risks in the fullest detail prior to surgery. - What is the follow up protocol?
Follow up is usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive visit restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a collar after surgery?
The type of collar and how long a patient must wear it depends upon the specifics of surgery and various other factors. This is decided by the surgeon and full guidance and training in the proper use of the collar are provided by the physiotherapy team. - How much pain will I have, and will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medications after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After discharge from hospital, this dressing must be kept clean and dry. Any soakage of the dressing should be reported through our Helpline number. Stitch removal is done by trained OT technicians at the patient’s residence. - Do I need to do the physical therapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific needs and need to be followed rigorously for the best results.

Dorsal/ Thoracic Spine (Back):
Lumber Spine (Low back):
The nerve roots that connect the lower part of the trunk and the lower limbs to the spinal cord and brain lie in the lumbar spinal canal. These nerves are responsible for power and sensation of the legs and the buttocks and genitalia along with the control of bladder, bowel and sexual functions.
Lumbar radiculopathy is often caused by a prolapsed disc causing low back pain with radiation to the leg/s. Pain may be associated with tingling, numbness, pins and needles like sensation and weakness of the leg/s. In most cases, the symptoms ease off gradually over several weeks with analgesics, good physiotherapy and normal activities. Surgery is an important option if the symptoms persist or progress.

FAQs:
- How many days do I need to stay in Hospital?
Patients are usually admitted to the hospital a day before surgery. After operation patients will be up and walking within the first day. If surgery is being done for leg pain due to nerve root compression, the pain improves significantly immediately following operation. Weakness or numbness, however, may take longer to improve. Patients are usually discharged on the 3rd day, allowing us to make sure that pain is well-controlled on oral medications and that the patient can move around indoors freely and without support prior to going home. - How long does this surgery take?
The time taken for surgery depends on each individual patient’s physical structure (e.g. height and weight) and diagnosis. The actual time needed for operation also depends on the number of levels to be decompressed and fused. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. Complications are rare, and, if they occur, usually mild. The risks of surgery include foot weakness, foot drop, infection, persistent pain after surgery, spinal nerve damage and tear of the sac around the nerves and problems in passing/holding urine and stool. There is also a risk that the level above or below the operated level will have an accelerated rate of degeneration. Around 10% of patients will have some temporary complications most of which are treatable and improve with time. Only 1% of patients may have some permanent deficits most of which will be of a trivial or minor nature. The risks of anaesthesia are largely dependent on the patient’s general physical health which will be investigated by the anaesthesiology team prior to surgery. The treating surgeon and anaesthesiologist will discuss these risks in the fullest detail during the pre-operative visit. - What is the follow up protocol?
Follow up visits are usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive follow up, restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a brace after surgery?
The style of brace and how long a patient must wear it, if at all, depends upon the specifics of surgery and various other factors. Usually, for a standard micro-lumbar discectomy, brace is not required. In fact, patients are advised to do the exercises as demonstrated by the physiotherapy team. - How painful will it be? Will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medication after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After discharge from hospital, this dressing must be kept clean and dry. Any soakage of the dressing should be reported through our Helpline number. Stitch removal is done by trained OT technicians at the patient’s residence. - Is there any need for physiotherapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific needs and need to be followed rigorously for the best results.
FAQs:
- How many days do I need to stay in Hopsital?
Patients are usually admitted to the hospital a day before surgery. After operation patients will be up and walking within the first day. If surgery is being done for leg pain due to nerve root compression, the pain improves significantly immediately following operation. Weakness or numbness, however, may take longer to improve. Patients are usually discharged on the 3rd day, allowing us to make sure that pain is well-controlled on oral medications and that the patient can move around indoors freely and without support prior to going home. - How long does this surgery take?
The time taken for operation depends on each individual patient’s physical structure (e.g. height and weight) and diagnosis. The actual time needed for operation also depends on the number of levels to be decompressed and fused. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. Complications are rare, and, if they occur, usually mild. The risks of surgery include foot weakness, foot drop, persistent pain after surgery, spinal nerve damage and tear of the sac around the nerves and problems in passing/holding urine and stool. There is also a risk that the level above or below the operated level will have an accelerated rate of degeneration. Infection and malposition or loosening of the screws are occasionally encountered. Around 10% of patients will have some temporary complications most of which are treatable and improve with time. Only 1% of patients may have some permanent deficits most of which will be of a trivial or minor nature. The risks of anaesthesia are largely dependent on the patient’s general physical health which will be investigated by the anaesthesiology team prior to surgery. The treating surgeon and anaesthesiologist will discuss these risks in the fullest detail during the pre-operative visit. - What is the follow up protocol?
Follow up is usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive follow up, restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a brace after surgery?
The style of brace and how long, if at all, a patient must wear it depends upon the specifics of surgery and various other factors. In this operation, the spine being fixed with screws and rods, the use of a brace is extremely rare. - How much pain will I have, and will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medications after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After discharge from hospital, this dressing must be kept clean and dry. Any soakage of the dressing should be reported through our Helpline number. Stitch removal is done by trained OT technicians at the patient’s residence. - Do I need to do the physical therapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific requirements and need to be followed rigorously for the best results.

FAQs: Please see Lumbar Decompression and Fixation (above)....
Removal of disc and bony outgrowths followed by placement of the spacer and bone graft are done as described for TLIF. The spacer restores the height between the bones, corrects the spinal curvature, and relieves pinched nerves. In some cases, where there is Osteoporosis and/or excessive degenerative changes the graft will need to be supported with metal plate and screws.

FAQs: Please see Lumbar Decompression and Fixation (above)....
Other Spinal Procedures:
The following conditions can potentially be treated using MIS Procedures:
- Degenerative disc disease.
- Herniated disc.
- Lumbar spinal stenosis.
- Spinal instability.
- Vertebral compression fractures.

FAQs:
- How many days do I need to stay in Hospital?
Patients are usually admitted to the hospital a day before surgery. After operation patients will be up and walking within the first day. If surgery is being done for leg pain due to nerve root compression, the pain improves significantly immediately following operation. Weakness or numbness, however, may take longer to improve. Patients are usually discharged on the 3rd day, allowing us to make sure that pain is well-controlled on oral medications and that the patient can move around indoors freely and without support prior to going home. - How long does this surgery take?
The time taken for operation depends on each individual patient’s physical structure (e.g. height and weight) and diagnosis. The actual time needed for operation also depends on the number of levels to be decompressed and fused. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. Complications are rare, and, if they occur, usually mild. The risks of surgery include foot weakness, foot drop, persistent pain after surgery, spinal nerve damage and tear of the sac around the nerves and problems in passing/holding urine and stool. There is also a risk that the level above or below the operated level will have an accelerated rate of degeneration. Infection and malposition or loosening of the screws are occasionally encountered. Around 10% of patients will have some temporary complications most of which are treatable and improve with time. Only 1% of patients may have some permanent deficits most of which will be of a trivial or minor nature. The risks of anaesthesia are largely dependent on the patient’s general physical health which will be investigated by the anaesthesiology team prior to surgery. The treating surgeon and anaesthesiologist will discuss these risks in the fullest detail during the pre-operative visit. - What is the follow up protocol?
Follow up visits are usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive follow up, restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a brace after surgery?
The style of brace and how long, if at all, a patient must wear it depends upon the specifics of surgery and various other factors. In this operation, the spine being fixed with screws and rods, the use of a brace is extremely rare. - How painful will it be? Will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medication after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After discharge from hospital, this dressing must be kept clean and dry. Any soakage of the dressing should be reported through our Helpline number. Stitch removal is done by trained OT technicians at the patient’s residence. - Is there any need for physiotherapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific needs and need to be followed rigorously for the best results.
Idiopathic- Where the exact cause is not known, these types of deformities grow rapidly during puberty.
Congenital- Where there is an abnormality in formation of vertebrae during the foetal stage which causes spinal deformity as the child grows.
Neuromuscular- Patient has a nerve or muscle disease that causes spinal deformities (for example- polio, cerebral palsy, or myelomeningocele). The uneven muscle pulls on the spine cause abnormal curvature.
Syndromic– Patient has a spinal deformity along with other symptoms which appear together (for example Marfan Syndrome, Retts syndrome, Ehler-Danlos syndrome).
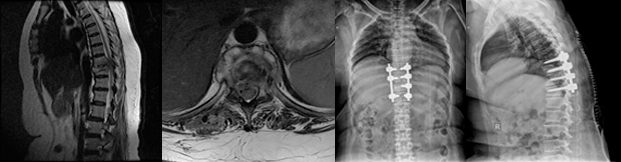
The patient usually presents with cosmetic disfigurement like uneven shoulders or waistline, a prominent chest wall on one side, hump on one side of the back, etc. These are the most common findings in a child with idiopathic scoliosis. It should be remembered that scoliosis other than idiopathic may present with weakness of arms or legs and loss of urinary control. A child with severe deformity may have difficulty in breathing due to impaired chest wall function.
Treatment protocols-
Following an extensive assessment, the doctor will decide to treat the condition with bracing or surgery depending on age, severity of curve, underlying disease processes and degree of breathing difficulty.
The treatment varies for each type of deformity. For idiopathic scoliosis surgery is usually done when the curve exceeds 40 degrees or in rapidly progressing curves. For other types of deformities surgery is done when child presents with pain, limb weakness, bladder disturbance and has achieved sufficient age and weight to sustain the operative procedure.
The surgical options are:
Posterior Fusion
Posterior fusion with instrumentation is the most common operation done for idiopathic scoliosis. In posterior fusion the spine is operated on from behind with an incision straight down the back. Various types of rods, hooks, wires or screws are used to partially straighten the spine and hold it fast while the bone fusion occurs.
Anterior Fusion
In anterior fusion, the spine is operated on from the front, or side. Anterior fusion is used in some special instances of idiopathic scoliosis. An incision is made along a rib and/or down the front of the abdomen to obtain access to the front of the spine. Bone graft from the hip, rib or bone bank is used for the fusion. Screws and washers attached to a rod may be used to straighten the spine.
Combined (Anterior and Posterior Fusion)
Some special cases of spinal deformity require both an anterior (front) and posterior (back) operation. Usually these can be done on the same day, but sometimes must be done at separate operations spaced 1-2 weeks apart.
These surgeries are performed under intraoperative neuro-monitoring system which gives continuous input to the surgeon about the function of the spinal cord throughout the surgery. This enables safe application of screws into the spine, bony correction and straightening of the deformed spine without risks of injuring the spinal cord.


FAQs:
- How many days do I need to stay in Hopsital?
Spinal deformity correction is major surgery. These are long duration surgeries which typically involve multiple levels of the spine. Some amount of pain may be expected after the surgery. The surgery and anaesthesiology teams, nursing staff and our physiotherapy team put a lot of emphasis on pain management to help the patient get up and about. Typically a patient needs about five to seven days to be able to sit, stand and walk. Usually before discharge from hospital a patient should be able to go to the toilet and climb stairs unaided. - How long does this surgery take?
Spinal deformity corrections are long surgeries which involve a coordinated team work of spine surgeons, anaesthesiologists, electro- physiologists, operation theatre technicians and nursing staff. It usually takes around 5-7 hrs. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. These complications are very few and infrequent. The risks of surgery include leg weakness, infection, screw malposition or loosening, nerve or spinal cord damage, tear of the sac around the nerves and bowel and bladder symptoms. Because of advancement in technology like neuro-monitoring, anaesthesia techniques, major improvement in screw design and operative instruments, these complications have come down significantly. Around 10% of patients will have some temporary complications most of which are treatable and improve with time. Only 1% of patients will have permanent deficits, many of which will be trivial. The risks of anaesthesia are largely based on the patient’s general physical health which will be investigated and managed by the anaesthesiologist prior to surgery. The treating surgeon and anaesthesiologist will discuss these risks in full detail at the pre-operative visit. - What is the follow up protocol?
Follow up is usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive follow up restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a brace after surgery?
The type of brace and how long a patient must wear it, if at all, depends upon the specifics of surgery and various other factors. If indicated, the treating surgeon will prescribe the particular brace required by the individual patient and the physiotherapy team will train and guide the patient in its use. - How much pain will I have, and will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medications after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. - How do I care for my surgical incision?
Once the surgery is over, we cover the incision with a sterile dressing. After discharge from hospital, this dressing must be kept clean and dry. Any soakage of the dressing should be reported through our Helpline number. Stitch removal is done by trained OT technicians at the patient’s residence. - Do I need to do the physical therapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific requirements and need to be followed rigorously for the best results.

FAQs:
- How many days do I need to stay in Hopsital?
Vertebroplasty and Kyphoplasty are one day procedures. Patients are usually admitted one day before the procedure. Usually the patient will be fit to go home the same day or next morning. Pain control is achieved with oral medication. - How long does this surgery take?
The time taken for surgery depends on the individual patient’s physical characteristics, diagnosis, and the number of levels to be treated. - Are there risks involved in this surgery?
There are risks and benefits of every medical and surgical intervention. These complications are very few and infrequent. The risks of surgery include cement leakage, pulmonary embolism, cerebrovascular and cardiovascular ischemia, potential nerve damage and urinary symptoms. There is also a risk that the vertebra above or below the operated one may develop another osteoporotic fracture. Around 10% of patients will have some temporary complications most of which are treatable and improve with treatment. Only 1% of patients may have permanent complications. The risks of anaesthesia are largely based on the patient’s general health which will be investigated and managed by the anaesthesiology team. The treating surgeon and anaesthesiologist will discuss these risks in the fullest detail prior to surgery. - What is the follow up protocol?
Follow up is usually scheduled at 1 month, 3 months, 1 year and 2 years post-surgery. In each successive visit restrictions are progressively relaxed and the patient is encouraged and guided to return to his/her normal life-style and activities. - Will I need a brace after surgery?
The type of brace and how long a patient must wear it depends upon the specifics of surgery and various other factors. The treating surgeon will prescribe the particular brace required by the individual patient and the physiotherapy team will train and guide the patient in its use. - How much pain will I have, and will I receive pain medications?
Every person has a different level of pain tolerance. Pain medications are, therefore, individualised for each patient and prescribed by our Anaesthesiology team. Full pain control is achieved with oral medications before discharge from hospital. - Do I need to take any other medications after the surgery?
In addition to pain medications, oral antibiotics are prescribed for one week. Patient will also be prescribed anti-osteoporotic medications depending on bone mineral density. - How do I care for my surgical incision?
Since Vertebroplasty and Kyphoplasty procedures are done using a narrow gauge needle, there are no stitches to care for or remove. - Do I need to do the physical therapy after surgery?
Our specialised physiotherapy team will advise and train every patient during the hospital stay. The regimen of exercises and manoeuvres are individually planned for the patient’s specific needs and need to be followed rigorously for the best results.
The recent advent of multidrug-resistant TB and also the tendency of TB to attack and spread rapidly in immunocompromised individuals have caused a setback in the management of the disease. At the same time great technical advancements and refinements in surgical techniques have provided tools for achieving what was hitherto considered impossible. The Spine Foundation has a huge and enviable record of success in the management of this dreaded condition.
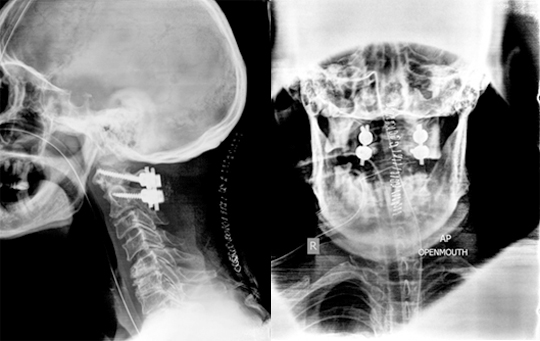
There are numerous disorders present at birth that affect the Craniovertebral Junction. These disorders may occur in isolation or be part of a generalised anomaly like Achondroplasia, Down Syndrome, Mucopolysaccharoidosis, Osteogenesis-Imperfecta, etc. Craniovertebral junction disorders may also occur later in life. They can result from motor vehicle accident, fall from a height, and certain disorders like Rheumatoid arthritis, Paget’sDisease, Ankylosing spondylitis etc. Various imaging methods like MRI, CT Scan, X rays are used for diagnosis.
Main goal of treatment is to maintain/provide spinal stability and to prevent neurological compression or trauma. Treatment depends on the exact nature of the disorder, duration of symptoms, age of the patient, degree of nerve compression, quality of bones and comorbidities, if any. Conservative management (cervical collars/braces/traction) is preferred in patients having mild symptoms without any evidence of compression of nerves and/or spinal instability. Surgery is reserved for patients with spinal instability and/or neurological symptoms.